SMART CLAIMS
SMART CLAIM
The Smart Claims solution automates health insurance claims adjudication. It includes automated data capturing and clinical enrichment, intelligent decision-making and fraud, waste and abuse (FWA) detection, as well as assessor screens with relevant information where complex manual review is recommended
It helps to automate and improve assessors’ review and decision-making whilst also preventing fraud in real-time using automated AI/ML models that detect anomalies, identify patterns of fraudulent behaviour and prevent human errors.
The solution is seamlessly integrated into the insurer’s claims system and deployed in their environment for claims decision recommendations (and controlled full automation) as well as real-time identification of current and historical anomalies.
The solution is seamlessly integrated into the insurer’s claims system and deployed in their environment for claims decision recommendations (and controlled full automation) as well as real-time identification of current and historical anomalies.
Key Features
OCR DATA CAPTURE
CLAIMS DECISION SUPPORT
FRAUD, WASTE AND ABUSE DETECTION
OUTLIER DETECTION
BENCHMARKING
AUTO-ADJUDICATION
Key Features
OCR DATA CAPTURE
CLAIMS DECISION SUPPORT
FRAUD, WASTE AND ABUSE DETECTION
OUTLIER DETECTION
BENCHMARKING
AUTO-ADJUDICATION
Smart Claims is an AI-powered technology solution that helps insurers deliver fast and accurate claims decisions.
> 500,000
claims processed
to date
Solution used by
more than half
of Singapore’s Shield Insurers
Entering
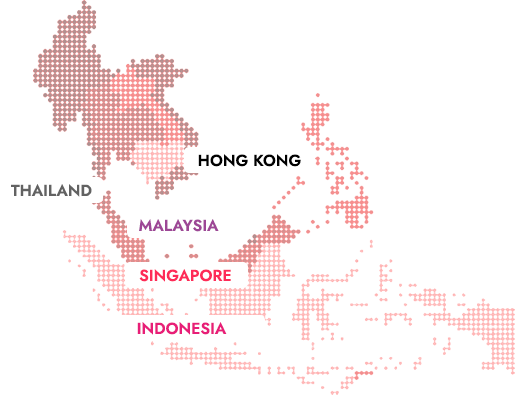
5
countries in
Southeast Asia + Japan
The Results?
Significant improvements in claims efficiency
and exceptional customer satisfaction.
Delighted customers
- 60% of all minor claims are paid within one working day
More efficient process
- 80% straight through processing and automation
- 60x faster assessment
Fraud detection and protected cashflow
- Identifies value-at-risk from FWA, typically 10 – 30% of the claims value
